TREATMENT OPTIONS
Fertility Treatments
Ovulation Induction (OI)
Ovulation Induction is one of the first treatments you may discuss with your doctor if you don’t ovulate naturally. Fertility medication can stimulate your ovaries and help them develop and release at least one egg.
This egg can then be fertilised naturally via sex, or through assisted conception with intrauterine insemination (IUI).1
OI is less invasive than other fertility treatments and the cost is lower because it does not require advanced technology.

- You take oral or injectable medication
- Your ovaries produce eggs
- Your eggs are released during ovulation
- The eggs are fertilised using timed sex or intrauterine insemination (IUI)


1 American Society for Reproductive Medicine (ASRM). Oral medicines for Inducing Ovulation. 2016. Available at: https://www.reprod uctivefacts.org/news-and-p ublications/fact-sheets-and-infographics/oral-medicines-f or-inducing-ovulation/?_t_id=3A8WKN Fk4nlhCtxXSaPCnA%3d%3d&_t_uuid=4bl nz4AzSKWuyBE8U2QHcA&_t_q=inducing+ov ulation&_t_tags=siteid%3adb69d13f-2074-4 46c-b7f0-d15628807d0c%2 clanguage%3aen%2c andquerymatch&_t_hit.id=ASRM_Models_Pages_Con tentPage/_dc6a15b5-47ce-4054 -9f4b-8ec2a536137c_en&_t_hit.pos=6. Accessed September 2023
2 American Society for Reproductive Medicine (ASRM). Side Effects of Injectable Fertility Drugs (Gonadotropins). 2012. Available at: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/side-effects-of-injectable-fertility-drugs-gonadotropins/?_t_id=3A8WKNFk4nlhCtxXSaPCnA%3d%3d&_ t_uuid=9Cv_8K_4S_mCvLA5zBp6IQ&_t_q=Side+ effects&_t_tags=siteid%3adb69d13f-2074-446c-b7f0-d15628807d0c%2clanguage%3aen%2candquerymatch&_t_hit.id= ASRM_Models_Pages_ContentPage/_7e9862b3-196a-41cb-97eb-cc12d41baffd_en &_t_ hit.pos=5. Accessed September 2023
3 Human Fertilisation & Embryology Authority. Fertility drugs. Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/fertility-drugs/. Accessed November 2022.
4 Holzer H et al., Fertil Steril. 2006;85(2):277-84.
5 Legro RS et al., New England Journal of Medicine. 2014; 371:119-129.
6Sawant S and Bhide P. Clinical Medicine Insights: Reproductive Health. 2019; 13:1179558119890867.
7 Katsikis I et al., Hippokratia. 2006; 10(3):120-127.
8 Practice Committees of the American Society for Reproductive Medicine and Society for Reproductive Endocrinology and Infertility. Fertility and Sterility. 2020; 113(1):66-70.
9 White DM et al., Reproduction. 2018; 156(1):F1-F10.
Intrauterine Insemination (IUI)
Intrauterine Insemination is a treatment where sperm is placed directly inside your uterus. It is often performed after inducing ovulation with fertility medication. Your doctor may recommend IUI as the first step in your fertility journey if you're diagnosed with unexplained infertility, experiencing male infertility or if you're using a donor sperm.

- The male partner has mild sperm abnormalities such as low sperm count or low motility
- You are using donated sperm, for example, single women and same sex couples It’s difficult to have sex, for example, because of a physical disability or psychosexual problems
- The man is HIV positive and his sperm needs to be washed before being used for fertilisation
- You have unexplained infertility (you will likely be recommended to undergo IUI with ovarian stimulation)
The IUI process explained
IUI is the most common form of artificial insemination3 and is a very simple procedure. Sperm is placed in the uterus using a fine catheter passed through the cervix when the woman is ovulating.4 Fertility medication can be used to stimulate ovulation before the IUI procedure.5 This treatment makes sure sperm is present in the uterus at the correct time and allows it to bypass the unfriendly, acidic environment of the vagina and cervix.
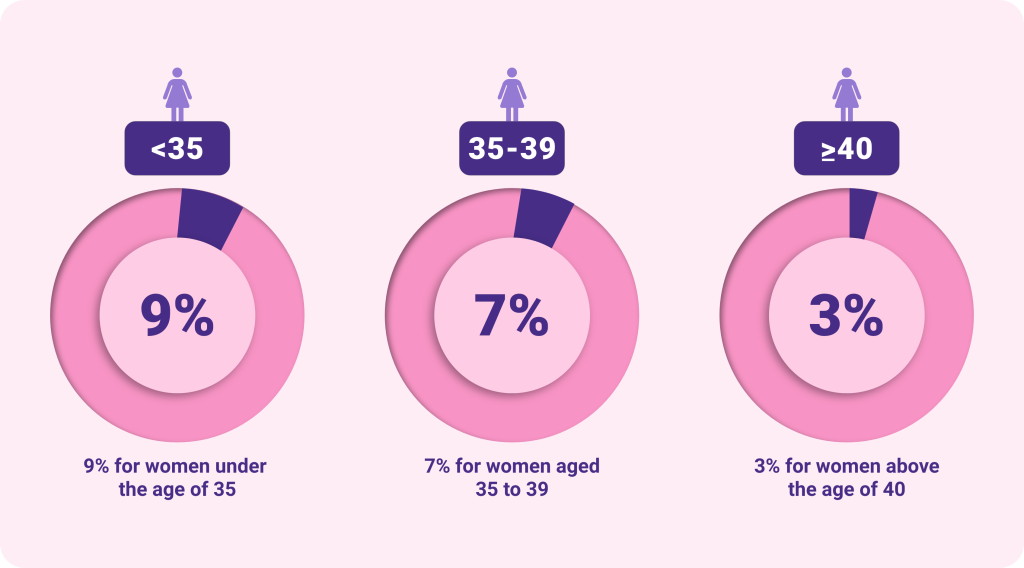
How successful is IUI?
For women undergoing IUI while taking fertility medication, the approximate percentage of cycles that result in a baby is dependent on their age:6 (insert image here) It’s important to be aware that many women need more than one round of IUI to achieve a successful pregnancy.1 This treatment makes sure sperm is present in the uterus at the correct time and allows it to bypass the unfriendly, acidic environment of the vagina and cervix.
The IUI journey7,8
01
Initial Consultation
This may be an underlying health problem such as infections, endometriosis and fibroids22.
02
Blood tests and investigations
03
Deciding your treatment plan
Day 2 or 3 of your menstrual cycle
Starting the IUI cycle
You will have an ultrasound and start taking ovulation induction medication if that’s part of your treatment plan. Regular ultrasounds will be performed to monitor your growing eggs and adjust your medication if necessary
Every 3 to 5 days
Monitoring
Regular ultrasounds will be performed to monitor your growing eggs and adjust your medication if necessary. You will administer the trigger shot to release your egg(s)
Day 8 to 12 of your menstrual cycle
Trigger injection
You will administer the trigger shot to release your egg(s).
After 2 weeks
Pregnancy blood test
You will have a blood test to determine if the treatment was a success and if you are pregnant.
Next steps
You will have ultrasounds to monitor the progress of your pregnancy or meet with your doctor to decide your next steps regarding further treatment.
1Human Fertilisation & Embryology Authority. Intrauterine insemination (IUI). Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/intrauterine-insemination-iui/. Accessed November 2022.
2 European Society of Human Reproduction and Embryology (ESHRE). ESHRE evidence-based guideline on Unexplained Infertility. 2023. Available at: https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Unexplained-infertility. Accessed July 2023.
3 Rachel Gurevich. Intravaginal, Intracervical and Intratubal Insemination. Verywell Family. 2021. Available at: https://www.verywellfamily.com/what-is-artificial-insemination-1960181. Accessed November 2022.
44. American Society for Reproductive Medicine (ASRM). Intrauterine insemination (IUI). 2016. Available at: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/intrauterine-insemination-iui/? _t_id=3A8WKNFk4nlhCtxXSaPCnA%3d%3d&_t_uui d=msnPUIj5TUGFY9CvKtd0Ng&_t_q=Intrauterine&_t_t ags=siteid%3adb69d13f-2074-446c-b7f0-d15628807d0c%2clanguage%3aen%2candquerymatch&_t_hit.id=ASR M_Models_Pages_ContentPage/_058cb5c8-038c-4d4b-b6b1-aa6d5b4a3e41_e n&_t _hit.pos=2. Accessed November 2022.
5 Victorian Assisted Reproductive Treatment Authority (VARTA). Fertility treatment explained. Available at: https://www.varta.org.au/fertility-treatment/fertility-treatment-explained#Types-of-treatment. Accessed November 2022.
6 The European IVF-Monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Human Reproduction Open. 2021; 2021(3): hoab026.
7 National Health Service (NHS). Intrauterine insemination (IUI). 2020. Available at: https://www.nhs.uk/conditions/artificial-insemination/. Accessed November 2022.
8 American Society for Reproductive Medicine (ASRM). Medications for Inducing Ovulation. 2016. Available at: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/oral-medicines-for-inducing-ovulation/?_t_id=3A8WKNFk4nlhCtxXSaPCnA%3d%3d&_t_u uid=GN6oBJbnTGuuwC1NfEDnyg&_t_q=+inducing+ovulation&_t_t ags=s iteid%3adb69d13f-2074-446c-b7f0-d15628807d0c%2 clanguage%3aen%2candquerymatch&_t_ hit.id=ASRM_Models_Pages_ContentPage/_dc6a15b 5-47ce-4054-9f4b- 8ec2a536137c_en&_t_hit.pos=5. Accessed November 2022.
In Vitro Fertilisation (IVF)
In Vitro Fertilisation is one of the well-known fertility treatments and is suitable for people with a wide range of fertility challenges. According to the European Society of Human Reproduction and Embryology (ESHRE), more than 10 million babies have already been born worldwide with the help of IVF.1
IVF is a complex process involving a series of fertility procedures at each step of the conception process. The defining feature of IVF is that the egg is fertilised outside the body in a lab, compared to IUI, where fertilisation occurs inside the body. The steps in IVF remove even more barriers that can stop the sperm from reaching the egg and gives your doctor more control over every stage of the process.2
If you have been trying to get pregnant for a long time already and other fertility treatments have not worked or are not suitable due to your or your partner´s condition, IVF could be an effective option to help you fulfil your dream of parenthood. Your doctor will help you decide if IVF is the right treatment for you.
Who is IVF suitable for?
Although most people with fertility problems (85–90%) can be treated using only medication or surgery,3 IVF can provide additional help for those still having trouble getting pregnant. This can be due to:4,5
Blocked or damaged fallopian tubes
Polycystic ovaries
Severe sperm abnormalities
Unexplained infertility where other treatments haven’t succeeded
Women who have difficulty ovulating and haven’t been successful with other treatments
Endometriosis
The IVF process explained
01
Controlling your menstrual cycle6
Down Regulation
To make your ovaries more receptive to the fertility hormones used in ovarian stimulation, your menstrual cycle will be controlled using hormonal injections which you administer daily at home. This is called down-regulation and the goal is to “inactivate” your ovaries for a short amount of time. Which day of your cycle you start this step and how long you take the medication for depends on the treatment protocol you and your doctor decide on. It may be the first stage of your treatment or may occur alongside. You may experience side effects such as hot flushes, night sweats, headaches, and mood swings, but they will improve once you stop taking the hormones.
02
Stimulating your ovaries7,8
Ovarian Stimulation
03
Part 1 Collecting your eggs7
Egg Retrieval Day
When your eggs are the right size, you will administer a hormonal injection which triggers your ovaries to fully mature your eggs to get them ready for collection. The injection replaces your body’s natural hormones that have been suppressed in the previous steps. Your doctor will decide which triggering option is best for you. Learn more about the trigger injection. You will be given an anaesthetic while your eggs are collected via transvaginal ultrasound aspiration. In this quick procedure, guided by an ultrasound probe, a thin needle connected to a suction device is inserted through the vagina wall into the follicles and eggs are removed. Depending on the number of eggs collected and your future plans, you might want to discuss freezing some of them with your doctor. You may experience abdominal pain/discomfort for a couple of days following the procedure. You might want to rest the following day to help recover from any pain or fatigue.
03
Part 2 Time to collect the sperm7
Sperm Collection
A semen sample is collected on the same day as the egg collection by masturbation. If the male partner is unable to ejaculate or has no sperm in his semen, a minor surgical procedure can be used to retrieve sperm directly from the testicles.
04
Eggs become embryos6,7
Fertilisation
An embryologist will preprare the sperm and eggs and combine them in the laboratory. The eggs will be placed in the sperm sample (conventional IVF) or individually fertilised using intracytoplasmic sperm injection (ICSI). An embryologist will check to see if any eggs have been successfully fertilised. These fertilised eggs are called zygotes, and they divide to become embryos. The embryo(s) will be nurtured and developed in an incubator that recreates the natural conditions of your uterus. Your embryo(s) will be monitored as they grow for 2 to 6 days.
05
It’s transfer day7,9
Embryo Transfer
06
Supporting your endometrium11
Luteal Phase Support
To help the embryo implant, during the luteal phase the hormone progesterone is given either as an injection, an oral tablet, a capsule, or a gel inserted into the vagina. Progesterone helps to thicken the uterus lining (endometrium), allowing the embryo to attach and grow. Your doctor will decide when to give progesterone following your egg collection to help prepare your uterus for the next steps.
Egg and embryo freezing
You should be aware that different countries have different rules about freezing embryos for future use.12 Whether to freeze unused eggs and embryos are decisions you might have to make during your IVF journey. Not every round of IVF is successful, and you may need multiple embryo transfers to achieve pregnancy. As an example, some women find that their uterus isn’t prepared to receive an embryo on the scheduled day of their transfer so freezing their developed embryos allows them to wait until their body is ready. You might hear this being referred to as a ‘freeze-all cycle’.13 Freezing eggs is also a choice you can make if you want to preserve your fertility and give yourself a better chance of having children later.
Preimplantation Genetic Testing for Monogenic Disorders (PGT-M) and Preimplantation Genetic Testing for Chromosomal Structural Rearrangements (PGT-SR)
Be aware that different countries have different rules on PGT-M and PGT-SR, in some they may be common practice but in others they can be restricted.12 Check with your doctor about the laws in your country. Some people are at risk of having a baby with a genetic disorder, for example, due to a family history of a serious genetic condition or a history of recurrent miscarriage due to chromosomal abnormalities. PGT-M and PGT-SR are techniques which might be recommended by your doctor to check some of your embryos’ cells for genetic or chromosomal abnormalities before they are transferred back into your uterus.15 PGT-M involves checking your embryos’ genes or chromosomes for a specific genetic condition. It can be used if there is a serious inherited disease in your family.15 PGT-SR involves looking for abnormalities in the structure of your embryos’ chromosomes. It can be used if you have a known chromosome structural rearrangement or have experienced multiple miscarriages due to chromosomal abnormalities.15 If you require PGT-M or PGT-SR, you will need to undergo IVF even if you do not have fertility problems because your embryos must be tested in a lab.
Pre-implantation Genetic Testing for Aneuploidy (PGT-A)
PGT-A means that before they are transferred into your uterus, embryos may be tested for abnormalities in the number of chromosomes. If an embryo has an abnormal number of chromosomes (called aneuploidy), it has less chance of developing into a baby. There is also a small chance it may result in a baby being born with a genetic condition.16 When testing for potential chromosomal abnormalities, an embryologist will carefully remove one or more cells from an embryo. The embryo will still develop normally with fewer cells.16 PGT-A is an invasive procedure for embryos which is largely restricted in some countries.14 Pre-implantation genetic testing is subject to the applicable local laws and can therefore be restricted or not allowed from country to country. It can only be performed in centres approved for pre-implantation genetic testing according to applicable local standards, after the approval of an interdisciplinary ethics committee and in accordance with generally accepted and latest state of science and techniques. For information relevant to your country, please check with your doctor.
PGT process
- Biopsies are taken from your embryos
- The samples are tested for abnormalities
- A genetic report is produced and reviewed by your doctor
- A healthy embryo is transferred to your uterus
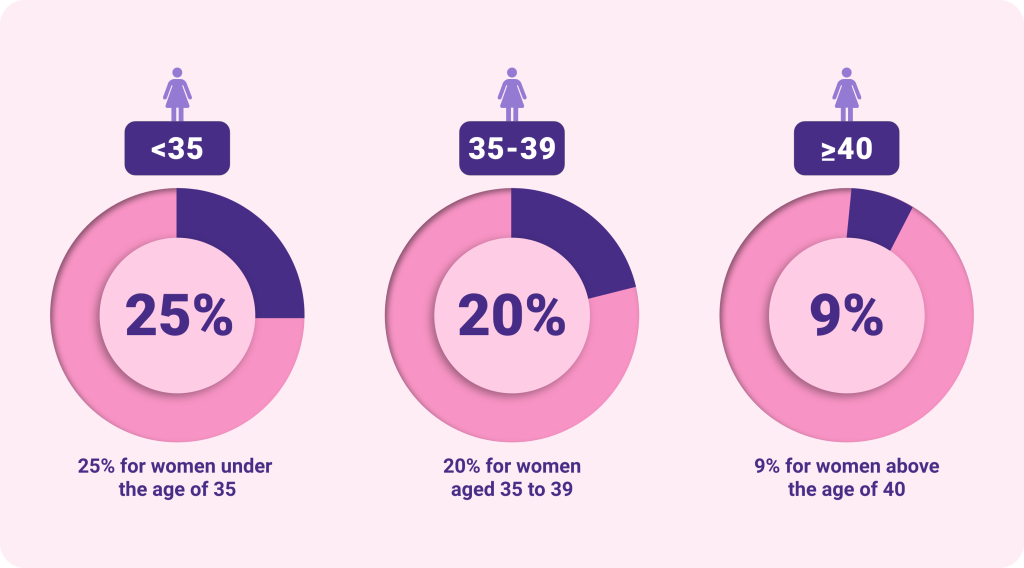
How successful is IVF?
Whilst it can be physically and emotionally demanding, IVF has been available for over 40 years and success rates have improved considerably during this time. The biggest factor in the success of IVF is a woman’s age. Success rates can vary greatly between women but for women using their own eggs, the average percentage of IVF cycles that result in a baby are:17 (insert image here)
1European Society of Human Reproduction and Embryology (ESHRE). ART fact sheet. Available at: https://www.eshre.eu/-/media/sitecore-files/Press-room/ESHREARTFactSheetv73.pdf. Accessed November 2023.
12. Human Fertilisation & Embryology Authority. Intrauterine Insemination (IUI). Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/intrauterine-insemination-iui/. Accessed November 2022.
3American Society for Reproductive Medicine (ASRM). Quick Facts About Infertility. 2017. Available at: https://www.reproductivefacts.org/browse-resources/frequently-asked-questions/faq-about-infertility/. Accessed November 2022.
4Human Fertilisation & Embryology Authority. In vitro fertilisation (IVF). Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/in-vitro-fertilisation-ivf/. Accessed November 2022.
5Fertility Society of Australia and New Zealand. IVF. Available at: https://www.fertilitysociety.com.au/ivf-treatment-australia-new-zealand/. Accessed November 2022
6. National Institute for Health and Care Excellence (NICE). Fertility problems: assessment and treatment, Information for the public. 2017. Available at: https://www.nice.org.uk/guidance/cg156/ifp/chapter/what-happens-in-ivf#step-1-down-regulation-of-the-ovaries. Accessed November 2022.
7 American Society for Reproductive Medicine (ASRM). Assisted Reproduction Technology – A Guide for Patients. 2018. Available at: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/assisted-reproductive-technologies-booklet/?_t_id=3A8WKNFk4nlhCtxXSaPCnA%3d%3d&_t_ uui d=73lCFuixRsmr2Zp2cCmfDg&_t_q=Assisted&_t_tags=si teid%3adb69d13f-2074-446c-b7f0-d15628807d0c%2clanguage%3aen%2candquerymatch& _t_hi t.id=ASRM_Models_Pages_ContentPage/_23a74fae-ee79-415c-bd20-386cc14b0a16_en&_t_hit.pos=2. Accessed November 2022.
8 American Society for Reproductive Medicine (ASRM). Medications for Inducing Ovulation. 2016. Available at: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/oral-medicines-for-inducing-ovulation/?_t_id=3A8WKNFk4nlhCtxXSaPCnA%3d%3d&_t_ uuid=GN6oBJbnTGu uwC1NfEDnyg&_t_q=+inducing+ovulation&_t_t ags=siteid%3adb69d1 3f-2074-446c-b7f0-d15628807d0c%2clanguage%3aen%2candquerymatch&_t_h it.id=ASRM_M odels_Pages_ContentPage/_dc6a15b5-47ce-4054-9f4b-8ec2a536137c_en&_t_hit.pos=5. Accessed November 2022.
9Human Fertilisation & Embryology Authority. Decisions to make about your embryos. Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/decisions-to-make-about-your-embryos/. Accessed July 2023.
10European IVF Monitoring Consortium (EIM), for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod Open. 2022 Jul 5;2022(3):hoac022.
11American Society for Reproductive Medicine (ASRM). Progesterone Supplementation During In Vitro Fertilization (IVF) Cycles. 2011. Available at: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/progesterone-supplementation-during-ivf/?_t_id=3A8W KNFk4nlhCtxXSaPCnA %3d%3d&_t_uuid=tejxnfDSQbe52g5tv9DBBg&_t_q=progeste rone+supplemen tation&_t_tags=siteid%3adb69d13f-2074-446c-b7f0-d15628807d0c%2clanguage%3aen%2candqueryma tch&_t_hit.id=ASRM_Models_ Pages_ContentPage/_ 3ac41084-342b-4811-a12e-532aa6526124_en&_t_hit.pos=2. Accessed November 2022.
12European Society of Human Reproduction and Embryology (ESHRE). Regulation and legislation in assisted reproduction. 2017.
13Human Fertilisation & Embryology Authority. Elective Freeze-all Cycles. Available at: https://www.hfea.gov.uk/treatments/treatment-add-ons/elective-freeze-all-cycles/. Accessed November 2022.
14The Embryo Protection Act. 2011. Available at: https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/Gesetze_und_Verordnungen/GuV/E/ESchG_EN_Fassung_Stand_10Dez2014_01.pdf Accessed September 2023
15 Human Fertilisation & Embryology Authority. Pre-implantation genetic testing for monogenic disorders (PGT-M) and Pre-implantation genetic testing for chromosomal structural rearrangements (PGT-SR). Available at: https://www.hfea.gov.uk/treatments/embryo-testing-and-treatments-for-disease/pre-implantation-genetic-testing-for-monogenic-disorders-pgt-m-and-pre-implantation-genetic-testing-for-chromosomal-structural-rearrangements-pgt-sr/. Accessed November 2022.
16Human Fertilisation & Embryology Authority. Pre-implantation genetic testing for aneuploidy (PGT-A). 2022. Available at: https://www.hfea.gov.uk/treatments/treatment-add-ons/pre-implantation-genetic-testing-for-aneuploidy-pgt-a/ Accessed: December 2022
17The European IVF-Monitoring Consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Human Reproduction Open. 2021; 2021(3):hoab026. 18. NHS. IVF – What happens. 2021. Available at: https://www.nhs.uk/conditions/ivf/what-happens/. Accessed November 2022.
Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic Sperm Injection (ICSI) is a procedure where a single sperm is directly injected into an egg to fertilise it. It is the most common and successful treatment to overcome severe male infertility.1 ICSI can also be used as fertility treatment in people with various other causes of infertility. For fertilisation to happen, a single sperm must enter the egg so that they can fuse together. Sometimes, the sperm is too slow or weak to break through the egg’s outer shell. In these cases, you may want to consider ICSI.
Who is ICSI suitable for?
Your doctor may recommend ICSI if…

The man:
- Has a very low sperm count (oligozoospermia)
- Has sperm with low movement or motility (asthenozoospermia)
- Has poor quality sperm (e.g. abnormally shaped sperm)
- Has blocked sperm ducts

- Has previously had IVF and none, or very few, of the eggs fertilised
- Is using donor or frozen sperm
- Is using frozen eggs
- ICSI is also becoming more popular for couples with unexplained infertility.2
The ICSI process explained
ICSI is a specialised form of IVF involving the same steps up until the moment the eggs are fertilised. Once the woman’s eggs have been collected and the man has provided a semen sample, the embryologist injects a single sperm directly into the centre of each mature egg.1 The fertilised eggs then develops into embryos and one or more are transferred into the uterus using the same steps as IVF.
How successful is ICSI?
With the help of ICSI treatment, it is possible to fertilise 50-80% of retrieved eggs. Once fertilisation takes place, the chance of having a baby via IVF is the same with or without ICSI.3
1Human Fertilisation & Embryology Authority. Intracytoplasmic Sperm Injection (ICSI). Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/intracytoplasmic-sperm-injection-icsi/. Accessed November 2022.
2Practice Committees of the American Society for Reproductive Medicine and Society for Assisted Reproductive Technology. Fertil Steril 2012;98(6):1395–1399.
3American Society for Reproductive Medicine (ASRM). What is Intracytoplasmic Sperm Injection (ICSI)? 2014. Available at: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/what-is-intracytoplasmic-sperm-injection-icsi/?_t_id=3A8WKNFk4nlhCtxXSaPCnA%3d%3d&_t_u id=KSukyYuuQymGpxVOK V5XBQ&_t_q=ICSI&_t_tags=siteid%3adb69d13f-2074-446c-b7f0-d15628807d0c%2clanguage%3aen%2candquerymatch&_t_ hit.id=A SRM_Models_Pages_Co ntentPage/_0e4ce974-11 8c-4fc5-b3eb-22662188ca05_en& _t_hit.pos=1. Accessed November 2022
What to expect during the treatment?
Undergoing fertility treatment isn’t easy. It’s important to be aware of what to expect and the challenges you might face along your journey. You can prepare for these challenges by understanding what you might experience and putting strategies in place to help you along the way.
Physical and Mental Changes
The hormones, medications, and procedures involved in fertility treatment can put a strain on your body and mind. This might cause physical and psychological impacts that can be challenging. Most of the changes occur in the first phase of treatment, during ovarian stimulation. They should subside not long after you have finished taking your prescribed medications.
Body
It’s not uncommon to experience weight changes when you’re taking hormone injections. They can also make you feel bloated, and you will likely develop soreness around the injection sites. Breast tenderness is also a common side effect during treatment.1
Mood
The additional hormones in your body can cause you to feel emotional and you may experience mood swings.1 Fertility treatment can also be a stressful and overwhelming journey which might heighten changes in your mood.
Appetite
The changes in hormonal balance caused by fertility medication can lead to an increased or decreased appetite in some people.2 You may also experience nausea, which could affect your appetite. In addition, constipation is a common side effect after an egg retrieval for IVF.3
Fatigue
It’s common to be left feeling exhausted because of changing hormone levels during fertility treatment. Specifically, an increased level of progesterone is often the cause of fatigue so you might feel particularly tired if you are given progesterone just before an embryo transfer to prepare your uterus for implantation.4
Injecting Fertility Hormones
If you are undergoing ovulation induction or IVF (in vitro fertilisation), or ICSI (intracytoplasmic sperm injection), you will need to inject fertility hormones at home. This may seem scary, especially if it’s your first time, but most people become comfortable with the injection process after some practice and are able to quickly incorporate it into their daily lifestyle.5 Some women prefer to give themselves the injections as this allows for scheduling flexibility because they need to be administered around the same time each day. Other women choose to ask for the help of their partner, a friend, or family member to administer the injections. There are two types of injections you may need to administer at home.
Subcutaneous
Subcutaneous injections are used to insert medication into the fat just under the skin. They are usually administered in the abdomen or thigh.
Intramuscular
Intramuscular injections insert medication deep into the muscle to allow it to be absorbed directly into your bloodstream. They are usually administered in the thigh or upper arm. You may feel overwhelmed and anxious about the responsibility of giving yourself the injections, but you will receive thorough training from a doctor or nurse beforehand. You will also be provided with leaflets or videos to refer to if you need to refresh your memory, so don’t worry too much about remembering every detail at first.
Understanding Treatment Risks
Fertility treatments are generally safe, but all medical procedures carry some risks.6 For most women, the chance of experiencing problems during pregnancy is the same whether they conceive naturally or through fertility treatments.6 It’s important to be aware of the potential complications and what to look out for to have a safe fertility journey and pregnancy. You can read about the most common risks associated with fertility treatment below.
Ovarian hyperstimulation syndrome
Ovarian hyperstimulation syndrome (OHSS) is an excessive response to the fertility hormones taken during ovarian stimulation which causes too many eggs to develop in the ovaries.7 This results in the ovaries becoming swollen and painful, causing symptoms like bloating, nausea, and feeling faint.6,7Mild OHSS can be treated at home with pain relief medication and rest. In rare cases, women can develop severe OHSS which can be life-threatening and requires hospital treatment; symptoms include stomach pains, vomiting, shortness of breath, and dehydration.6,7 If you develop any of the symptoms of mild or severe OHSS you should contact your doctor immediately.
Multiple births
Women undergoing fertility treatment are more likely to fall pregnant with multiple babies (twins, triplets, or more). Fertility hormones taken during treatment encourage your ovaries to grow multiple eggs, increasing the chance of more than one egg fertilising. IVF in particular carries a very high risk for multiple births if more than one embryo is transferred to the uterus in a cycle. For this reason, in Europe it’s most common to transfer one embryo per cycle,8 but this can differ depending on your medical history and country regulations. Most multiple pregnancies result in healthy babies and mothers, but you should consider the risk of multiple births when deciding on your treatment plan with your doctor.
Ectopic pregnancy
An ectopic pregnancy is when the embryo implants and develops outside of your uterus, usually in the fallopian tubes.6 This occurs in 1-2% of pregnancies in the general population, but the risk increases to 2-5% if you undergo IVF treatment because there’s a chance the embryo will travel to the fallopian tube after being transferred to your uterus.9 After your embryo transfer you should look out for symptoms of an ectopic pregnancy which include low abdominal pain on one side, vaginal bleeding, and diarrhoea or pain when you go to the toilet.6 If you develop any of these symptoms you should contact your doctor immediately.
Birth Defects
Research suggests that there is a small increased risk of birth defects in babies born following IVF treatment compared to naturally conceived babies. In the general population around 4% of babies are born with birth defects. This rises to 5-6% in babies born via IVF.9 It is not known exactly what causes this increased risk, but it may be due to parental characteristics such as age and cause of infertility.10 It’s not clear whether babies born after ICSI have an added risk of birth defects compared to those born after conventional IVF.10
1Rachel Gurevich. Side Effects and Risks of Fertility Drugs. Verywell Family. 2020. Available at: https://www.verywellfamily.com/what-are-the-potential-risks-of-fertility-drugs-1960190. Accessed March 2023.
2Michael Bihari. Why Progesterone Is Used During IVF. Verywell Family. 2021. Available at: https://www.verywellfamily.com/can-i-use-vaginal-progesterone-during-ivf-1124028 Accessed March 2023.
3Sara Lindberg. How to Find Relief from Constipation After Egg Retrieval. Healthline. 2022. Available at: https://www.healthline.com/health/constipation-after-egg-retrieval Accessed March 2023
4Drugs.com. Progesterone Side Effects. 2022. Available at: https://www.drugs.com/sfx/progesterone-side-effects.html Accessed March 2023.
5Rachel Gurevich. How to Give Yourself a Subcutaneous Injection. Verywell Family. 2021. Available at: https://www.verywellfamily.com/how-to-give-yourself-a-subcutaneous-injection-1960196. Accessed April 2023.
6Human Fertilisation & Embryology Authority (HFEA). Risks of fertility treatment. Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/risks-of-fertility-treatment/ Accessed March 2023.
7American Society for Reproductive Medicine (ASRM). Ovarian Hyperstimulation syndrome (OHSS). 2014. Available at: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/ovarian-hyperstimulation-syndrome-ohss/?_t_id= 3A8WKNFk4nlhCtxXSaP CnA%3d%3d&_t_uuid= lIwJwKzjT0Ga4zbeu 08PHg&_t_q=OHSS&_t_t ags=siteid%3adb69d13f-2074 -446c-b7f0-d15628807d0c%2clanguage%3aen%2candquerymatch&_t_ hit.id=ASRM_Mod els_Pages_ContentPage/_a86aa141-bc3f-4bcf-bc96-4595f132561b_en&_t_hit.pos=2 Accessed March 2023.
8European IVF Monitoring Consortium (EIM), for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod Open. 2022 Jul 5;2022(3):hoac022
9Athanasiou et al. J Immunological Sci. 2020 Jan;4(1):1-5.
10 Victorian Assisted Reproductive Treatment Authority (VARTA). Possible health effects of IVF. 2016. Available at: https://www.varta.org.au/sites/default/files/2020-12/Possible%20health%20effects%20of%20IVF.pdf Accessed March 2023.